Slowing the transmission of COVID-19 will give health care facilities a better chance of serving all the people who need help and reducing the number of fatalities. Graphic courtesy of Matthew McQueen, Director of the Public Health Program at the University of Colorado.
No school for three weeks, only days to plan for it, and no group activities as we engage in social distancing. It could be a parent’s nightmare. And it’s real in Denver. Maybe you’re thinking you’re one of the lucky ones with grandparents nearby—but read to the end before you ask them. They are the ones being protected by the school closings.
Statistics from China showed children and young people contracted COVID-19 at very low rates, according to a StatNews article by Sharon Begley. As of Feb. 11, 1.2% of the cases were aged 10 to 19 and only one had died. “ In fact, through mid-January, zero children in Wuhan, the epicenter of the outbreak, had contracted Covid-19. It’s not clear whether that’s because children do not show signs of illness even if infected.” ….By contrast the fatality rate for people 80 and over was 14.8%.
To help us understand the crisis we’re in and why we need to make significant changes in our lives, we asked a public health expert and journalists with technical knowledge for permission to share some of their current work. Find links to their articles at the end.
Closing schools has a huge impact on families. Why was such a dramatic step necessary?
Reducing the rate of transmission is critical, writes the Director of the Public Health Program, Matthew McQueen at the University of Colorado Boulder in an article on ScienceAlert.com. “Rather than letting the virus quickly rampage through the population and burn itself out fast, the idea is to spread all those infections out over a longer period of time.
“Yes, it would potentially prolong the epidemic. But in doing so, public health agencies and the health care infrastructure gain invaluable time to respond to the crisis.
“Most importantly, ‘flattening the curve’ provides an opportunity to significantly reduce deaths from COVID-19.”
A rapid rise of the epidemic puts “a tremendous burden on health care providers – many of whom will fall ill themselves and be forced to self-isolate, becoming unable to provide care for those in need….demand for patient care will outpace capacity – things like the number of hospital beds, ventilators and so on – for a significant amount of time.
“So yes, even if every person on Earth eventually comes down with COVID-19, there are real benefits to making sure it doesn’t all happen in the next few weeks….
“To be clear, social distancing comes with a substantial economic cost as people aren’t engaged in the same work and life activities that fuel the economy as they were just a month or two ago,” writes McQueen.
On days when parents are struggling most in this new world we’re living in, remembering the consequences to the health care system, as described in the StatNews article by Helen Branswell, may help:
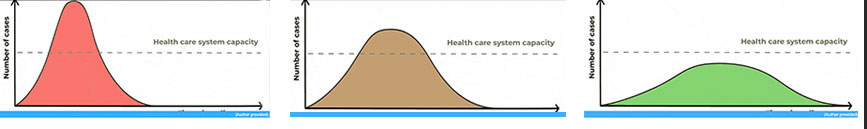
Slowing the transmission of COVID-19 will give health care facilities a better chance of serving the people who need help and reducing the number of fatalities. Image created from graphic provided by Matthew McQueen, Director of the Public Health Program at the University of Colorado.
“On any normal day, health systems in the United States typically run close to capacity. If a hospital is overwhelmed by Covid-19 cases, patients will have a lower chance of surviving than they would if they became ill when the hospital’s patient load was more manageable. People in car crashes, people with cancer, pregnant women who have complications during delivery — all those people risk getting a lesser caliber of care when a hospital is trying to cope with the chaos of an outbreak.
“I think the whole notion of flattening the curve is to slow things down so that this doesn’t hit us like a brick wall,” said Michael Mina, associate medical director of clinical microbiology at Boston’s Brigham and Women’s Hospital. “It’s really all borne out of the risk of our health care infrastructure pulling apart at the seams if the virus spreads too quickly and too many people start showing up at the emergency room at any given time.”
Alessandro Vespignani, director of the Network Science Institute at Northeastern University, is gravely worried about what he’s hearing from contacts in Italy, where people initially played down the outbreak as “a kind of flu,” he said. Hospitals in the north of the country, which the virus first took root, are filled beyond capacity, he said, and may soon face the nightmarish dilemma of having to decide who to try to save.
Vespignani, along with colleagues, published a recent modeling study in Science that showed travel restrictions — which the United States has adopted to a degree — only slow spread when combined with public health interventions and individual behavioral change…. “I think people are not yet fully understanding the scale of this outbreak and how dangerous it is to downplay,” he said.
What do the statistics from China tell us about the impact on older people?
The following section of a StatNews.com article by Sharon Begley, “Who is getting sick, and how sick? A breakdown of coronavirus risk by demographic factors” offers a look how different ages of people were impacted in China:
The new coronavirus is not an equal-opportunity killer: Being elderly and having other illnesses, for instance, greatly increases the risk of dying from the disease the virus causes, Covid-19. It’s also possible being male could put you at increased risk.
For both medical and public health reasons, researchers want to figure out who’s most at risk of being infected and who’s most at risk of developing severe or even lethal illness. With that kind of information, clinicians would know whom to treat more aggressively, government officials would have a better idea of steps to take, and everyone would know whether they need to take special, additional precautions.
Here’s what research has shown three months into the outbreak:
The vast majority of cases in China — 87% — were in people ages 30 to 79, the China Center for Disease Control reported last month based on data from all 72,314 of those diagnosed with Covid-19 as of Feb. 11. That probably reflects something about biology more than lifestyle, such as being in frequent contact with other people. Teens and people in their 20s also encounter many others, at school and work and on public transit, yet they don’t seem to be contracting the disease at significant rates: Only 8.1% of cases were 20-somethings, 1.2% were teens, and 0.9% were 9 or younger. The World Health Organization mission to China found that 78% of the cases reported as of Feb. 20 were in people ages 30 to 69.
The death toll skews old even more strongly. Overall, China CDC found, 2.3% of confirmed cases died. But the fatality rate was 14.8% in people 80 or older, likely reflecting the presence of other diseases, a weaker immune system, or simply worse overall health. By contrast, the fatality rate was 1.3% in 50-somethings, 0.4% in 40-somethings, and 0.2% in people 10 to 39.
The age-related death risk probably reflects the strength, or weakness, of the respiratory system. About half of the 109 Covid-19 patients (ages 22 to 94) treated at Central Hospital of Wuhan, researchers there reported, developed acute respiratory distress syndrome (ARDS), in which fluid builds up in the small air sacs of the lungs. That restricts how much air the lungs can take in, reducing the oxygen supply to vital organs, sometimes fatally; half of the ARDS patients died, compared to 9% of patients who did not develop the syndrome.
The ARDS patients had an average age of 61, compared to an average age of 49 for those who did not develop ARDS. Elderly patients “were more likely to develop ARDS,” the researchers wrote, suggesting how age can make Covid-19 more severe and even fatal: age increases the risk that the respiratory system will basically shut down under viral assault.
Youth, in contrast, seems to be protective. The WHO mission reported a relatively low incidence in people under 18, who made up only 2.4% of all reported cases. In fact, through mid-January, zero children in Wuhan, the epicenter of the outbreak, had contracted Covid-19. It’s not clear whether that’s because children do not show signs of illness even if infected.
Even cases among children and teens aged 10 to 19 are rare. As of Feb. 11 there were 549 cases in that age group, 1.2% of the total, China CDC found. Only one had died.
One intriguing explanation for the apparent resilience of youth: in regions near Hubei province, young children seem especially likely to be exposed to other coronaviruses, scientists in China reported in 2018. That might have given them at least partial immunity to this one.
The Front Porch thanks these three authors and their publications for sharing their work to give our readers a better understanding of why fundamental changes are necessary in their lives at this time:
- “Who is getting sick, and how sick? A breakdown of coronavirus risk by demographic factors,” by Sharon Begley, StatNews.com https://www.statnews.com/2020/03/03/who-is-getting-sick-and-how-sick-a-breakdown-of-coronavirus-risk-by-demographic-factors/
- “This One Graph Shows Why ‘Flattening The Curve’ Is So Critical For COVID-19 Right Now,” by Matthew McQueen, Director of the Public Health Program at the University of Colorado Boulder, ScienceAlert.com.
https://www.sciencealert.com/dragging-out-the-coronavirus-epidemic-is-important-in-saving-lives# - “Why ‘flattening the curve’ may be the world’s best bet to slow the coronavirus,” by Helen Branswell, StatNews.com
https://www.statnews.com/2020/03/11/flattening-curve-coronavirus/

0 Comments